How to Avoid the Change of Tibial Posterior Inclination during HTO Operation
 Oct. 19, 2020
Oct. 19, 2020
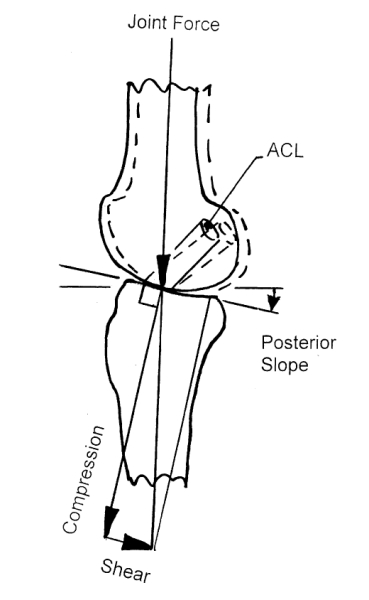
High tibial osteotomy (HTO) can correct the coronal force line, but the resulting changes in the sagittal tibia posterior angle also cause widespread concern.
After tibial osteotomy, the sagittal plane often has too large or too small a tibial posterior angle, which will affect the function of the anterior and posterior cruciate ligament, affect the height of the patella (significant correlation), cause knee joint instability, and affect the long-term effect of HTO.
Some studies believe that the change of tibia posterior angle is not only related to the amount of coronal correction but also related to surgical technique.
Incomplete posterior medial cortical osteotomy, incomplete posterior medial soft tissue release, rotation of metaphysis around hinge points in the process of distraction, equal anterior and anterior distraction of osteotomy and anterior plate fixation all lead to changes in posterior inclination Angle, affecting long-term results.
1. Measurement of the posterior inclination of the tibial plateau before surgery
Measured by the tibial anatomical axis, the normal range of tibia posterior angle of Chinese is 10.8° (SD3.5°), but there are big differences between individuals, so effective preoperative measurement is very important.
The knee joint is fully extended, the femoral condyles are completely overlapped, and tibia rotation should be avoided to obtain true lateral x-rays. At the same time, strict measurement methods are used. The accuracy of the tibial posterior inclination measurement may reach 1°-4°.
2. The position of the outer hinge
Studies have shown that compared with standard hinges, the use of low hinge positions for osteotomy may increase the risk of lateral hinge fractures and significantly increase the tibial posterior angle.
3. Complete osteotomy and soft tissue loosening
Incomplete osteotomy of the posterior cortex of the tibia or partial loosening of the posterior soft tissue will affect the azimuth angle of the two hinge points, resulting in abnormal posterior angle after closed HTO.
For open HTO surgery, due to the limitation of the medial collateral ligament, the osteotomy area may be spread more anteriorly during expansion, thereby increasing the posterior inclination of the tibial plateau. Therefore, care should be taken to ensure that the surface of the medial collateral ligament has long fibers (especially the posterior medial) that have been fully released.
4. Prediction of the open gap
Observed from the cross-section, the anteromedial cortex of the proximal tibia is oblique or triangular, and it is approximately 45° with the posterior cortex.
The lateral cortex is more perpendicular to the posterior edge of the tibia; therefore, an open wedge osteotomy with the same anteroposterior space can increase the posterior inclination of the tibia.
In contrast, the lateral closed wedge osteotomy with equal anteroposterior space along the lateral tibial cortex has a relatively small effect on the tibial posterior angle.
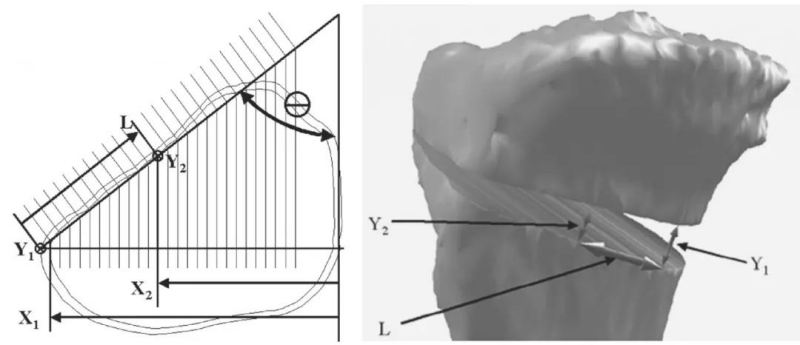
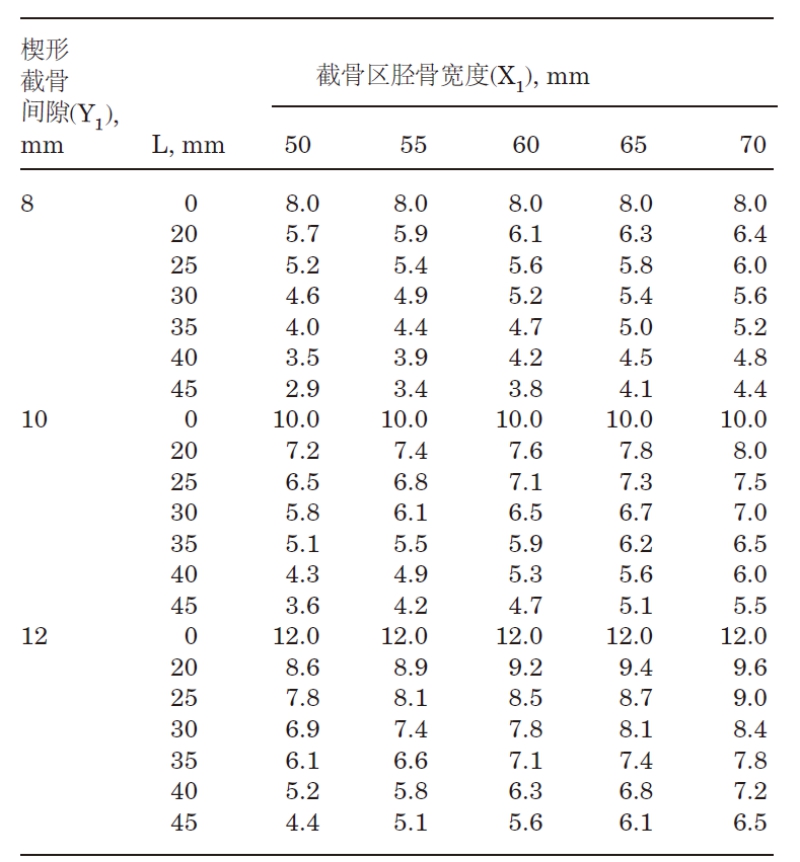
Studies have shown that if the anterior distraction gap (tibial tubercle) is about half of the posterior distraction gap, TPS can be maintained. It is recommended to expose the posterior cortex of the tibia to evaluate the anterior and posterior space or refer to the following diagram: L=(X1-X2)/sin (θ); Y2=(X2)(Y1)/X1
5. Fixed position
Studies have shown that the fixed position is significantly related to the change of the posterior angle (P<0.001). Regardless of the plate length, the position of the anterior and middle plate will increase the posterior inclination of the tibia (P<0.05). Rodner et al. found that for patients undergoing OWHTO (8° preoperatively), when the plate is placed in the middle of the anterior medial ridge of the tibia, the posterior inclination angle increases to 14°. It is suggested that the inner middle and rear 1/3 position can better achieve structural stability and safety.
The above information is provided by the joint prosthesis supplier.













